Te Whakapūkōwhaitanga: he whakahoutanga i runga anō i ngā taunakitanga
Kua mātaitia e mātou ētahi taunakitanga hou e pā ana ki te whakapūkōwhaitanga o te wai, i tāia i muri i te putanga mai o tā Te Apārangi pūrongo i te tau 2014. E rārangi mai nei ko tā mātou i kite ai.
Ka puta māori noa te pūkōwhai i te wai, otirā, ka taea tana whakakaha i te niho, ka taea hoki tana ārai i te pakohu niho. I Aotearoa, i te nuinga o te wā, he iti iho te pūkōwhai ka puta māori noa mai i te wai, tēnā i te nui e tika ana e rangona ai ēnei painga hauora ā-waha. Me te aha, hei kōkiritanga hauora tūmatanui, ka āpitihia atu te pūkōwhai ki ngā tini puna wai kia whakapiki i te nui o te pūkōwhai o roto. E āminetia ana tēnei mahi e te tini o ngāi ringarehe hauora, heoi anō, me tino mārama tonu tātou ki ngā tūraru ka whai pānga pea ki te whakapikinga ake o te nui o te pūkōwhai ka tau ki ō tātou tinana.
I puta i a Te Apārangi [1] tētahi arotakenga whānui i te tau 2014 e aro nei ki ngā pānga ā-hauora o te whakapūkōwhaitanga wai [2]. E ai ki te arotakenga rā, i ngā taumata o te whakapūkōwhai i te wai ka whāia i Aotearoa, karekau he pānga kino e whai tikanga ana i hua ake i te pūkōwhai. Kua tirohia e mātou ētahi rangahau hou e pā ana ki te whakapūkōwhaitanga, me ētahi arotakenga whānui nō muri mai tāia ai, ā, ko tā mātou, e tika tonu ana ngā whakatau whakamutunga a Te Apārangi.

Image credit: Kurt:S/Flickr (CC BY-SA 2.0).
Ngā kitenge matua
- Kāore te hauora ā-niho e hāpaitia e te pūkōwhai ka puta māori noa mai i te wai i Aotearoa, inā hoki, he iti rawa.
- Ko te nui o te pūkōwhai ka whai wāhi atu ai te tangata e hāngai ana ki ana whiringa kai, ki te nui o te wai ka inumia, ki te nui o te pūkōwhai i te wai, otirā ki ana hātepe akuaku ā-waha.
- E whai hua tonu ana te āpitihanga o te pūkōwhai ki te wai i runga i tana whakaheke i te nui o ngā pakohu niho i Aotearoa, ā, he āhuatanga tēnei e tino whai tikanga ana ki te whai kia tautika ake ai ngā tatauranga hauora o te iwi, hāunga te taumata ohapori.
- Ki te nui rawa te pūkōwhai ka kainga, ka hua pea ko te ‘fluorosis’ ā-niho (arā, he makenu pakiri ā-niho i puta ai he kōtingotingo puata-kore i ngā niho). Heoi anō, i runga tonu i ngā taumata o te whakapūkōwhaitanga o te wai i Aotearoa, kāore i kino te pāngia (arā, karekau he āwangawanga ā-hauora, he iti noa, karekau rānei he āwangawanga ā- tirohanga nei), ka mutu, i te nuinga o te wā, hanga ōrite ana te nui o ngā kēhi mate pūkōwhai ā-niho ka kitea i ngā wāhi kua whakapūkōwhaitia te wai, me ērā kāore i pērātia.
- Arā ētahi, he nui ake te pūkōwhai ki a rātou i tērā e tika ana e rangona ai ngā hua hauora ā-waha, ina koa ko ngā kōhungahunga ka whāngaia ki te miraka kua mahia ki te paura rāwekeweke, otirā e noho ana ki ngā wāhi kua whakapūkōwhaitia te wai. Nā te pēnei, ka nui ake pea te tūraru ka wāhi pāngia rātou e te ‘fluorosis’ ā-niho, engari karekau he pākinotanga hauora i tua atu e whakapaetia ana.
- E whakaatuhia tonutia ana e ngā rangahau nō nā tata nei, ki te tino nui rawa, ki te auau hoki te whai wāhi atu ki te pūkōwhai, ka hua pea ko ētahi pānga kino ā-whanaketanga roro, ā-hirikapo anō hoki. Heoi anō, i runga i ngā taumata o te whakapūkōwhaitanga o te wai i Aotearoa, ehara tēnei i te take e māharahara ai tātou.
Contents
- The purpose of this webpage
- What did the Aotearoa New Zealand 2014 review find?
- Dental caries is a serious problem in Aotearoa New Zealand
- Why do we add fluoride to water?
- How does fluoride help teeth?
- Review of health impacts
- Fluoride exposure and intake
- Further reading and resources
- Peer reviewers
- Footnotes
The purpose of this webpage
This webpage provides an accessible summary of a comprehensive report published in 2014 by the Royal Society Te Apārangi, Health effects of water fluoridation: A review of the scientific evidence [3], which was prepared jointly with the Office of the Prime Minister’s Chief Science Advisor. This webpage may be used by various professionals and by people who are interested in taking a closer look at the evidence base. The focus of this work is on scientific evidence, rather than the ethics or philosophy of public health measures, though we acknowledge this is an ongoing source of discussion (see for example, Awofeso (2012) [4], Jiang et al. (2014) [5] and Song and Kim (2021) [6]).
The webpage also provides an update on key research on fluoridation published subsequently, as well as comprehensive reviews undertaken internationally (namely in Australia and draft outputs from the United States). We have not repeated the work undertaken in 2014 but have updated it using the same sources.
We have looked at the significance of this research in the context of Aotearoa New Zealand, particularly in relation to current and proposed fluoridation levels in community water supplies and other exposures to fluoride.
This information is additional to that provided by the New Zealand Government, for example see the Fluoride Facts website and Ministry of Health webpages (see Fluoride and Oral Health and Water Fluoridation).
The content has been peer-reviewed by subject-matter experts (see our list of reviewers).

What did the last review in Aotearoa New Zealand find?
A comprehensive report was published by the Royal Society Te Apārangi, prepared jointly with the Office of the Prime Minister’s Chief Science Advisor, Health effects of water fluoridation: A review of the scientific evidence. The review was undertaken in 2014 and revised in January 2015.
The report concluded:
Given the caveat that science can never be absolute, the panel is unanimous in its conclusion that there are no adverse effects of fluoride of any significance arising from fluoridation at the levels used in New Zealand. In particular, no effects on brain development, cancer risk or cardiovascular or metabolic risk have been substantiated, and the safety margins are such that no subset of the population is at risk because of fluoridation… Our assessment suggests that it is appropriate, from the scientific perspective, that fluoridation be expanded to assist those New Zealand communities that currently do not benefit from this public health measure – particularly those with a high prevalence of dental caries.
There are no adverse effects of fluoride of any significance arising from fluoridation at the levels used in New Zealand
Dental caries is a serious problem in Aotearoa New Zealand
Aotearoa New Zealand has poor oral health in the population despite improvement over the last few decades. [7]
Dental caries (also known as tooth decay or dental cavity) remain the most prevalent chronic disease in Aotearoa New Zealand affecting all people of all ages and are worst among Māori and Pasifika people. As Treaty partners and under the United Nations Declaration on the Rights of Indigenous Peoples, the Crown has a commitment to achieve equity in health outcomes, including in oral health, for Māori. [8]
The cause of dental caries occurs when bacteria present in the mouth feeds on sugary food eaten by individuals to create acids that attack the protective layers (enamel and dentin) of teeth. As the enamel and dentin weaken and lose minerals, a cavity is formed (see Figure 1).

Figure 1: Example of tooth decay in front teeth of upper jaw (primary teeth). Credit: Phantumvanit P. Source: WHO.
When this cavity or tooth decay is not detected early for treatment then problems of pain and tooth ache arise, and this can lead to a lack of sleep, not eating well, and missed school or work. If the tooth decay is not treated early enough this can potentially result in the affected tooth being removed. This can cause further issues, both aesthetically and not being able to chew food properly.
Incidence of poor oral health in children is also a significant concern. For example, in Auckland and Northland 41% of children aged five had one or more decayed teeth that had been filled or removed because of dental cavities (see Figure 2).
In 2019/2020, 7% of adults (over 15 years old) who participated in the New Zealand Health Survey had a tooth removed due to decay within the past year of being surveyed. Almost half of adults [9] have had one or more teeth removed in their lifetime due to either decay, an abscess, infection, or gum disease.
In addition, less than half of adult New Zealanders had visited a dental healthcare worker in the past year and only 62% reported brushing their teeth twice a day with fluoride toothpaste.


Figure 2: Dental decay in five-year-olds in Auckland and Northland. Data from Aung et al. (2019). [10]
Why do we add fluoride to water?
In many countries, including Aotearoa New Zealand, natural levels of fluoride in water are not high enough to provide the health benefits described in the section below ‘How does fluoride help teeth?’. Consequently, here and throughout the world many water supplies have fluoride added so that levels are high enough to provide oral health benefits to the population (see for example, in Australia, the United States, and Canada) (see Figure 3).

Figure 3: Proportion of the population given government-regulated fluoridated water (light teal 0–33%, teal 34–67%, black 68–100% of population). From Johnston and Strobel (2020). [11]
Conversely, some countries have very high levels of fluoride (see Figure 4) in their water supplies either because of natural occurrence or because of industrial contamination (some of these countries include India, Estonia, China, and parts of South Africa). Where levels of fluoride in water supplies exceed recommended limits, some water supplies may have fluoride removed to lower content to recommended levels.
Throughout the world, water is a common vehicle for adding fluoride to increase intake, but as an alternative some countries add fluoride to salt instead. This happens in several countries in Western Europe [12] (including Switzerland [13], Germany [14], and France [15]), as well as other countries such as Mexico [16]. Young children and infants have a very low fluoride intake from fluoridated salt as their intake of salt is low, so there are some drawbacks in using salt rather than water as a vehicle for increasing fluoride in the diet. Ingesting fluoridated salt alone would not be sufficient to reach the level of fluoride required to gain oral health benefits. Aotearoa New Zealand does use salt to deliver other public health benefits – for many decades iodine has been added to table salt to prevent goitre (this disease was previously very common in parts of the country).

Figure 4: Map showing the occurrence and distribution of fluoride in groundwater in different parts of the world. From Kimambo et al. (2019). [17]
Is fluoridation an effective health measure in Aotearoa New Zealand?
Evidence of the effectiveness of fluoridation of water supplies to mitigate dental caries has been accumulating for over 60 years. Aotearoa New Zealand water supplies generally have naturally low concentrations of fluoride because of low levels in the environment. [18] When water is fluoridated in Aotearoa New Zealand it involves adding fluoride to reach levels between 0.7 and 1.0 mg/L. It reduces both the prevalence of dental caries in the population and the severity of dental caries in individuals who are affected. In Aotearoa New Zealand, there are significant differences in decay rates in communities with fluoridated and non-fluoridated water supplies, despite most people also using fluoridated toothpaste. [19] As levels of tooth decay are highest among the most deprived socioeconomic groups, this is also the part of the population which will have the greatest benefits from water fluoridation.
Key evidence for the benefits of fluoridation on oral health can be drawn from the 2009 New Zealand Oral Health Survey. [20] The survey interviewed almost 5,000 children and adults, and included dental examinations of almost 3,200 of the participants. This was the first survey in Aotearoa New Zealand that collected comprehensive and nationwide information on the oral health of children (aged 2–17 years). Decayed, missing and filled teeth is one of the key measures used to determine oral health. Differences in this measure between fluoridated and non-fluoridated areas can be seen in Figure 5, which shows that children living in non-fluoridated areas have 1.7 times as many decayed, missing or filled teeth than those in fluoridated areas.

Figure 5: The adjusted ratio of means of decayed, missing or filled teeth per person, among children (aged 2–17 years old), by fluoridation status (adjusted by age, sex, ethnic group, and index of deprivation) data from Ministry of Health. [21]
The most recent local data is still drawn from the 2009 survey. For comparison, the Australian review undertaken in 2017 found that water fluoridation reduces tooth decay in children and adolescents by 26% to 44%, and by 27% in adults. [22] A summary of the Australian review is available here.
Royal Society Te Apārangi concludes that fluoridation of water supplies is the most effective public health measure for the prevention of dental decay. This is despite the majority of people also using fluoridated toothpaste.
Does fluoridation help decrease health inequities?
As with many other health issues, levels of tooth decay are highest among the most deprived socioeconomic groups, of which Māori and Pacific peoples predominate. Royal Society Te Apārangi conclude that these communities are also those which will have the greatest benefits from water being fluoridated. [23] Consequently, fluoridation of drinking-water is expected to reduce health inequities.
In 2016, a New Zealand peer-reviewed study explored potential ethnic inequities in dental health in relation to water fluoridation. [24] The study looked at children aged between 5 and 12–13 years old between 2004–2013. The study found that Māori children in areas with community water fluoridation had better oral health profiles than Māori children in non-fluoridated areas; however, Māori children continue to carry a disproportionate oral health burden than non-Māori. [25]

Figure 6: Adjusted odds ratios from the final multivariable model of severe caries experience reported in Schluter et al. (2020). [29]
Several papers have been published that analysed national cross-sectional data collected as part of the ‘B4 School Check’ screening programme. The screening programme provides data on a near complete cohort of children aged four years old (first implemented in 2008 though not universal until 2010). [26] The first study using this data to analyse dental health, published in 2018, analysed data from 2010–2016. [27] The study found there were differences in the prevalence of dental caries depending on socioeconomic status evident by four years of age. The worst dental caries experience and steepest socioeconomic gradients were observed among Māori and Pacific children. Another study analysing this data considered severe dental caries and found that fluoridation of drinking-water continues to be associated with a reduced prevalence of severe dental caries in four year old children. [28] There are significantly higher levels (around 21%) of severe dental caries in areas without water fluoridation once age, sex, ethnicity, area-level deprivation and residential location are accounted for. Deprivation and ethnicity can have compounding effects – Figure 6 provides examples of this in the rate of caries for children of different ethnicities and deprivation levels.
In 2020, a study was published that looked at the relationship between water fluoridation and children’s hospital visits for dental treatment that could have been provided earlier by primary care (e.g. GP, dentist). [30] The study found an association between fluoridation of drinking-water and reduced dental hospital visits for children up to 12 years old. This effect was greatest for children living in the most deprived areas and indicated a greater health gain from fluoridated drinking-water for those most socio-economically disadvantaged. This means decisions on fluoridation of drinking-water can contribute to structural inequities in oral-health outcomes for children.
Compared to non-Indigenous people, a high proportion of Māori rate their oral health as fair or poor, have more untreated dental caries or missing teeth, and fewer teeth that have been restored. [31] Historically, Māori have had poor access to dental care and while the involvement of Māori and Pacific health providers in policies affecting oral health has improved over the years, further effort is still necessary to continue reducing inequalities in oral health. [32] The Quality Improvement Group for Māori oral health providers is one such group that is contributing to improving oral health outcomes for Māori.
Fluoridation continues to be a critical oral health measure, in part because it is effective in improving oral health regardless of parental knowledge of early childhood oral care.
Spotlight on fluoridation in Aotearoa New Zealand
In Aotearoa New Zealand, some of our reticulated water supplies (i.e. the water networks that provide the majority of New Zealanders with tap water) are fluoridated so that levels of fluoride are high enough to provide these health benefits to the population. Currently, approximately 60% of the total population drink water from fluoridated water supplies (see ESR map of fluoridated water supplies). A cost-benefit analysis of water fluoridation in Aotearoa New Zealand concluded that fluoridation of community water supplies remained a highly cost-effective health measure. [33]
Legislation and codes of practice provide:
- the recommended fluoride content for drinking-water in Aotearoa New Zealand,
- guidelines on the design and operation of water fluoridation plants, and
- sampling and monitoring requirements. This legislation is important to provide assurance that fluoridation is occurring at safe levels.
The decision to fluoridate reticulated water supplies is currently made by local authorities, under their duty to ‘improve, promote, and protect public health’ within their district.
In 2016, the Health Minister announced that he would introduce legislation to have District Health Boards, rather than local authorities, decide which community water supplies would be fluoridated, given that fluoridation is a health-related issue. The Government is currently proposing to move this decision-making power to the Director-General of Health instead (which would be made by way of Supplementary Order Paper). The Health (Fluoridation of Drinking Water) Amendment Bill was introduced in November 2016 and is currently awaiting its second reading.
There appears to generally be public support for water fluoridation among those who voted on the issue. For example, recent referendums have indicated majority support for water fluoridation (see Hamilton (68%), Hastings (63%) and Whakatāne (60%) in 2013 and Thames (73%) in 2015). In the 2009 Oral Health Survey, 42% of participants were strongly or somewhat supportive of water fluoridation, while only 15% were strongly or somewhat opposed to water fluoridation (as reported in Whyman et al. (2016) [34]).
Fluoridation remains a topic of public interest and concern, [35] from dark humour in fiction (see Dr Strangelove’s proclamation of fluoridated water as a communist plot [36]), to various action groups (such as Fluoride Free NZ), to researchers with legitimate concerns about high exposures to fluoride (see, for example, recent article on pros and cons of fluoridation [37]). The current potential legislative developments have heightened public interest.
Sampling and monitoring of water supplies
There are standards and guidelines in Aotearoa New Zealand that set out how high fluoride levels can be in water and how it should be added, sampled and monitored (see Aotearoa New Zealand legislation and guidelines). Where fluoridation of a water supply is undertaken, drinking-water leaving the treatment plant must be sampled (for fluoride) at least weekly under the water supplier’s monitoring programme (under the Drinking-water Standards for New Zealand 2005). Long-term exposure to very high levels of fluoride can have negative health impacts so it is important that the systems used to add, sample and monitor fluoride addition are reliable and trusted.
In recent years, there have been significant issues with some water supplies (unrelated to fluoride). For example, the large scale campylobacteriosis outbreak in Havelock North that was associated with untreated reticulated water. [38] Events such as this can create concerns about water quality. However, there do not appear to have been any issues related to fluoride reported. ESR reports on compliance with the Drinking-water Standards (see map here). Compliance is based on how a water treatment plant meets requirements over a 12-month period. No compliance issues related to fluoride were reported in the most recent publicly available reporting period (2018/2019).
How does fluoride help teeth?

Figure 7: Illustrative figure of how fluoride impacts teeth.
The enamel of your teeth is made of mainly hydroxide, calcium and phosphate ions, a structure called hydroxyapatite. Fluoride reacts strongly with these ions in developing teeth and results in strong teeth with enamel that is more resistant to decay. [39] In this reaction, fluoride replaces hydroxide, converting hydroxyapatite to fluorapatite.
These fluorapatite crystals are more symmetric and stack better than the hydroxyapatite crystals (see Figure 8).
With topical exposure through fluoridated toothpaste and other sources (including water), fluoride is found throughout the mouth, including in saliva and plaque fluid, and bound to soft tissues (like your gums, tongue and cheeks) and enamel (see Figure 7, above). With consistent exposure, this reduces the rate at which enamel demineralises (i.e. when tooth decay is occurring) and also promotes remineralisation. [40]
The greatest effect of fluoride in reducing tooth decay comes from ongoing topical exposure, though benefits are maximised if there is also system exposure while the teeth are forming. [41]

Figure 8: Illustrative figure of how fluoride affects tooth enamel.
Review of health impacts
Fluoride is naturally found in the environment and can have broad benefits for oral health. It helps to strengthen teeth and provides protection against dental decay.
If we have an adequate intake of fluoride, we can gain these oral health benefits. However, if we have too much fluoride it can cause negative health impacts (which is also true of many commonly consumed minerals and vitamins that provide health benefits).
What is dental fluorosis?
Dental fluorosis is a tooth enamel defect, which is typically observed as opaque white spots on the enamel.
Excessive exposure to fluoride while teeth are forming in the jaw can cause dental fluorosis (a tooth enamel defect, which is typically observed as opaque white spots on the enamel). Mild dental fluorosis can present a potential cosmetic concern (from the appearance of the white spots on teeth) but no health concern. However, more severe forms of dental fluorosis can cause discoloured, pitted or weakened teeth.
As tooth development occurs in the first eight years of life, children are not susceptible to fluorosis past this age.

Figure 9: An example of mild dental fluorosis (CC BY-NC-ND 4.0) from Cavalheiro et al. 2017.
Is fluorosis a concern here?
Most dental fluorosis occurring in Aotearoa New Zealand is mild and there has been no severe case of fluorosis reported here.
As reported by Royal Society Te Apārangi in 2014, most dental fluorosis occurring in Aotearoa New Zealand is mild and there has been no severe case of fluorosis reported here. [42] While prevalence of mild dental fluorosis generally increases with fluoridation of water, there are usually other factors contributing more significantly to increasing risk (for example, young children regularly swallowing fluoridated dental products). Formula-fed babies are more likely to be at higher risk of mild dental fluorosis when the water supply is fluoridated.
Have there been any recent developments?
There is little difference in fluorosis between areas of fluoridated and non-fluoridated water supplies.
Key information on the prevalence of dental fluorosis in Aotearoa New Zealand still relies on the 2009 New Zealand Oral Health Survey. This survey examined interviewees between the ages of 8-30 years (who had retained some of their natural teeth) to assess presence and severity of dental fluorosis (the scale used is shown in Figure 10). Dental fluorosis was only assessed in people in this age bracket as it is harder to separate fluorosis from other changes in tooth appearance in adults (such as the tooth enamel maturing and dental procedures like fillings and crowns). As can be seen in Figure 11, there is little difference in the prevalence of dental fluorosis in areas of fluoridated water supplies and those without it at the population-level. This shows that dental fluorosis occurs regardless of whether water supplies are fluoridated, and that the addition of fluoride to water supplies has no significant effect on the number of people who experience fluorosis. The majority of participants had no form of dental fluorosis present, while most of those with fluorosis present had questionable or very mild forms (see Figure 10) and studies have shown that fluorosis can decrease over time. No severe cases were reported.
Similar results have also been found in Australia, which has a similar approach to water fluoridation as Aotearoa New Zealand. The 2016 NHMRC Evidence Evaluation found almost all dental fluorosis occurring in Australia is very mild or mild, doesn’t affect the function of the teeth, and is not of aesthetic concern to those who have it. There is no significant difference in the incidence of dental fluorosis between fluoridated and non-fluoridated areas and fluorosis has declined over the time in which fluoridation of community water in Australia expanded. The decline is linked to reduced exposure to fluoride from other sources (e.g. availability and promotion of low fluoride toothpaste for children, public health messages and guidelines about use of fluoridated health care products).
Changes in the incidence and severity of dental fluorosis at a population level can serve as an indicator of over-exposure to fluoride. [43] This can be important where there is potential concern of more serious impacts.

Figure 11: Prevalence and severity of dental fluorosis in Aotearoa New Zealand in 2009 (see 2009 New Zealand Oral Health Survey).

Figure 10: Categories of dental fluorosis used in the 2009 New Zealand Oral Health Survey (see methodology report).
Could fluoride have possible neurodevelopmental and cognitive health effects?
As summarised by Royal Society Te Apārangi in 2014 [44], in studies on rats, extremely high doses of fluoride have been associated with various deficits in learning and behaviour following prolonged exposure. These doses are orders of magnitude higher [45] than what humans are exposed to through drinking water at levels used in fluoridation of water supplies in Aotearoa New Zealand.
In humans, there have been a number of reports of an association between very high water fluoride levels and reduced IQ. Many of the studies have been of low quality. Royal Society Te Apārangi concluded in their 2014 report [46] that while there is some evidence that very high fluoride concentrations may have a possible, slight adverse effect on developing brains, there is no convincing evidence of neurological effects at fluoride concentrations achieved by fluoridation of water supplies in Aotearoa New Zealand.
A 2015 study followed a cohort of more than 1,000 people born in the early 1970s in Dunedin, data from this study was used to examine the association between community water fluoridation and IQ. [47] This includes both prenatal exposure and exposure throughout childhood. This study did not find evidence that water fluoridation in Aotearoa New Zealand affects neurological development or IQ. Royal Society Te Apārangi considered this to be a relatively high-quality study.
Further summary and analysis of studies undertaken pre-2015 can be found in the Royal Society Te Apārangi report.
Have there been any recent developments?
In 2017, the Australian NHMRC review considered studies available at the time that had found associations between higher fluoride concentrations and possible neurological effects. The Australian review’s reference group was confident that the body of evidence at that time was valid, applicable to the Australian context, and demonstrated no association between water fluoridation and the cognitive function or IQ of children or adults.
Several studies published in other countries recently have found associations between higher prenatal or childhood fluoride exposure and cognitive outcomes (see for example, Mexico [48], China [49], and Canada [50]). There have also been multiple meta-analyses and reviews performed (see resources and further reading below). Recent discussion around fluoride has mainly focused on epidemiological studies (i.e. studying populations with different exposures) rather than experimental studies (i.e. undertaken with animals in labs). Experimental studies show that expected every-day human exposure to fluoride still falls well below the levels that lead to adverse effects in animals. [51]
The Australian review’s reference group was confident that the body of evidence at that time was valid, applicable to the Australian context, and demonstrated no association between water fluoridation and the cognitive function or IQ of children or adults.
Most epidemiological studies reporting reduced IQ at higher fluoride exposures do not sufficiently consider the influence of confounding factors [52] as these can be very difficult to control or consider. This means that results found can often be due to confounding factors rather than what the study is considering (e.g. the association between fluoride and neurodevelopmental and cognitive outcomes).
Many studies finding potential associations between fluoride and cognitive outcomes are of lesser relevance to Aotearoa New Zealand’s context due to these countries having much higher fluoride exposure levels and other environmental differences (like the presence of higher levels of lead or arsenic in water supplies). However, the Canadian study was of greater potential concern because the conditions in which it took place are more comparable to Aotearoa New Zealand. Similar to the study undertaken in Aotearoa New Zealand, the Canadian study also followed a birth cohort (taking a group of children born within a certain time period and following them as they age) and compared the IQ of children between fluoridated and non-fluoridated areas.
The study undertaken in Canada [53] found that the mother’s exposure to fluoride during pregnancy was associated with lower IQ scores [54] in boys (but not girls), even at optimally fluoridated water levels (i.e. between 0.7-1.2 mg/L). If this finding were replicated in robust studies, it would potentially be concerning as Aotearoa New Zealand recommends fluoridation of water between 0.7 and 1.0 mg/L. There was significant and valid criticism of aspects of the study by many subject-matter experts when it was released (see for example, ‘expert reaction to study looking at maternal exposure to fluoride and IQ in children’). The study used sub-group analysis to find an association that is not explained in the paper (i.e. why were only boys affected [55] and why verbal IQ was not impacted), the effect appeared to be driven by the minority of participants that had much higher fluoride exposures (i.e. higher than those in Aotearoa New Zealand).
The results found in the study undertaken in Canada [56] are also in contrast to those found in the study undertaken in Aotearoa New Zealand [57], which has the advantage of more accurately reflecting local contextual factors. These are the only two studies published since 2012 that have looked at the effects of fluoride on IQ in areas where water is precisely fluoridated as a public health measure, as opposed to the majority of studies where fluoride was naturally present in water supplies [58]. A recent review by Guth et al. (2020) [59], evaluated evidence for human developmental neurotoxicity from fluoride [60], and discussed some of the differences between the two studies (summarised in table [will be in a dropdown]). Though difficult to compare directly due to differing methodologies, the Broadbent et al. (2015) study has many advantages: a larger and more complete birth cohort, a more robust method of measuring intelligence [61]; and consideration of significant cofounders such as birthweight and breastfeeding.
Comparison of prospective studies undertaken on impacts of fluoridation on IQ, adapted from Guth et al. (2020)
Comparison of prospective studies undertaken on impacts of fluoridation on IQ, adapted from Guth et al. (2020)
| Broadbent et al. (2015) [61] | Green et al. (2019) [56] | Comments | |
|---|---|---|---|
| Location | Dunedin, Aotearoa New Zealand. | Canada | The Broadbent et al. (2015) study is more directly applicable to our environmental context, having been undertaken in Aotearoa New Zealand. |
| Study size | Near complete birth cohort of 1037 children (91% of eligible births), followed for 38 years (born between 1972–1973). | 610 mother-child pairs (from 2001 pregnant women participating in the MIREC programme) (born between 2008–2012). | Both studies had significant numbers, although Broadbent et al. (2015) had a more complete birth cohort and higher number of participants. |
| Fluoridation | The majority (around 90%) of study members lived in areas with community water fluoridation. Fluoridated areas (0.7–1.0mg/L), non-fluoridated (0.0–0.3mg/L). | Less than half (around 40%) of study members lived in areas that with community water fluoridation. Fluoridated areas (mean 0.59mg/L), non-fluoridated (mean 0.13mg/L). | The Broadbent et al. (2015) study had a relatively small sample of participants in non-fluoridated areas compared to fluoridated areas. |
| Measurement of IQ | IQ was measured at multiple points between 7 and 13 years old, and at 38 years old. | IQ was measured in children once, between 3 and 4 years old. | The IQ of children improves quite rapidly between the ages of 3 and 4 years, which is a limitation in the Green et al. (2019) study as children’s exact age at time of test is not considered in the statistical analysis. Broadbent et al. (2015) used a more robust measure of IQ by undertaking multiple assessment across different ages (7, 9, 11, 13) and averaging results. |
| Measurement of fluoride intake | Fluoride intake estimated via drinking water, fluoride toothpaste and fluoride tablets. | Maternal urinary fluoride (MUF) was measured for 512 of the pregnant women, and self-reported maternal daily fluoride intake from water and beverage consumption was available for 400 pregnant women. | In Green et al. (2019), the study used creatinine-adjusted urinary fluoride concentrations to account for urinary dilution – this could cause bias if a study participant suffered from renal problems influencing the IQ. As indicated by the authors (Broadbent et al. 2015), a limitation of the study is the fact that individual water intake level was not directly measured and dietary fluoride was not considered. |
| Confounding factors | Adjustment for potential confounding variables, including sex, socioeconomic status, breastfeeding, and birth weight. | Green et al. (2019) did not consider breastfeeding and low birth weight as possible confounders (both factors significantly associated with IQ in the study of Broadbent et al.); they considered some of the relevant confounders (city, socioeconomic status, maternal education, race/ethnicity, prenatal second-hand smoke exposure), but did not adjust for others (alcohol consumption and further dietary factors, other sources of fluoride exposure, exact age of children at time point of testing). | Broadbent et al. (2015) studied the influence of possible confounding factors and obtained significant associations of socioeconomic status, breastfeeding, and low birth weight with the IQ. These factors were used to adjust the analysis of community water fluoridation with IQ. As indicated by the authors (Broadbent et al. 2015), a limitation of the study is the fact that individual water intake level was not directly measured and dietary fluoride was not considered. |
| IQ of parents | Educational attainment used as proxy for adult IQ outcomes. | No parental IQ data. | Limitation as parental IQ is a strong confounder. IQ could also potentially influence level of fluoride exposure. |
| Results | No clear differences in IQ because of fluoride exposure were noted. These findings held after adjusting for potential confounding variables. | Male children show a decrease in IQ with increasing maternal urinary fluoride concentration, while female children show a non-significant increase. | The male-specific association identified by Green et al. (2019) is not easily explained and was not replicated in Broadbent et al. (2015). |
The review by Guth et al. (2020), considers that current epidemiological evidence does not provide sufficient arguments to raise concerns with regard to fluoridation of drinking-water (in the range of 0.7-1.0 mg/L). Guth et al. state that: “In conclusion, based on the totality of currently available scientific evidence, the present review does not support the presumption that fluoride should be assessed as a human developmental neurotoxicant at the current exposure levels in Europe.”
However, despite criticism, the Canadian study does create further uncertainty in the body of evidence as can be seen in the recent draft review documents produced by the US Department of Health and Human Services National Toxicology Program (NTP) regarding fluoride exposure and neurodevelopmental and cognitive health effects (see Section below).
US review of evidence: Ongoing review process of draft outputs on neurodevelopmental and cognitive health effects
In 2019, the US Department of Health and Human Services released a Draft National Toxicology Program (NTP) Monograph on systematic review of fluoride exposure and neurodevelopmental and cognitive health effects for the purposes of peer review. The NTP states that the draft does not represent and should not be construed to represent any NTP determination or policy.
The NTP requested that the National Academies of Sciences, Engineering, and Medicine review the draft monograph. The draft has been reviewed and a second revision of the draft has subsequently been reviewed in late 2020. Concerns raised during reviews of the draft monograph included that much of the evidence presented in the review came from studies that involved high fluoride concentrations, whereas there was little or no conclusive evidence about the effects of fluoride at lower exposures (e.g. less than 1.5 mg/L in drinking water).
While not yet finalised, the draft concludes that fluoride is presumed to be a cognitive neurodevelopmental hazard, based on evidence from populations where drinking-water has fluoride concentrations of more than 1.5 mg/L.
A circulating draft, revised 16 September 2020 (which the NTP stressed is for the purpose of pre-dissemination peer review and does not represent and should not be construed to represent any NTP determination or policy) concludes that:
…when considering all the evidence, including studies with exposures to fluoride levels higher than 1.5 mg/L in water, NTP concludes that fluoride is presumed to be a cognitive neurodevelopmental hazard to humans. This conclusion is based on a moderate level of evidence that shows a consistent and robust pattern of findings in human studies across several different populations demonstrating that higher fluoride exposure (e.g., >1.5 mg/L in drinking water) is associated with lower IQ and other cognitive effects in children.
While not yet finalised, the draft concludes that fluoride is presumed to be a cognitive neurodevelopmental hazard, based on evidence from populations where drinking-water has fluoride concentrations of more than 1.5 mg/L. This determination is very clearly dose dependent. The extent to which water fluoride concentration impacts on daily fluoride intake obviously depends on diet (see discussion below on fluoride intake and exposure). The National Academies of Sciences, Engineering and Medicine review of the draft concluded that:
As documented in this letter report, the committee had difficulty in following various aspects of the reported methods, identified a few worrisome remaining inconsistencies, was not able to find some key data used in the meta-analysis, and had concern about the wording of some conclusions. Even though the evidence provided appears to show consistent indications of an association between exposure to high fluoride concentrations and cognitive deficits in children, the monograph falls short of providing a clear and convincing argument that supports its assessment. It also needs to emphasize that much of the evidence presented comes from studies that involve relatively high fluoride concentrations and that the monograph cannot be used to draw conclusions regarding low fluoride exposure concentrations (less than 1.5 mg/L), including those typically associated with drinking water fluoridation.”[…] NTP therefore should make it clear that the monograph cannot be used to draw any conclusions regarding low fluoride exposure concentrations, including those typically associated with drinking-water fluoridation.
The exposure to fluoride for individuals varies according to both water intake and dietary exposure. This is explored in the section on how we’re getting fluoride and where we’re getting it from.
What does this mean for Aotearoa New Zealand?
In Aotearoa New Zealand, drinking-water is fluoridated between 0.7 mg/L and 1.0 mg/L and thus it is unlikely that intake would reach the higher levels that have limited evidence of association with lower IQ or other cognitive effects in children (see Figure 19). Additionally, the significant epidemiological life course study undertaken in Aotearoa New Zealand [62] has not shown evidence of IQ or other cognitive effects in children due to fluoride exposure.
The conclusion reached by Royal Society Te Apārangi remains appropriate. While there is some evidence that high fluoride concentrations may have an adverse effect on developing brains, there is no convincing evidence of neurological effects at fluoride concentrations achieved by fluoridation of water supplies in Aotearoa New Zealand.
While there is some evidence that high fluoride concentrations may have an adverse effect on developing brains, there is no convincing evidence of neurological effects at fluoride concentrations achieved by fluoridation of water supplies in Aotearoa New Zealand.
Cancer
Concerns have been raised about whether consuming fluoridated water could increase the risk of cancer, in particular bone cancer (osteosarcoma) because fluoride is deposited into bones. Multiple systematic reviews have concluded that based on the best available evidence, fluoride (at any level) could not be classified as a human carcinogen. In 2014, the Royal Society Te Apārangi concluded that based on the available evidence there is no significant risk of cancer arising from fluoridation of water supplies.
There are no significant subsequent developments to report. Recent studies have not found associations between fluoridation and: osteosarcoma in the United States; secondary bone cancer in New York; childhood/adolescent osteosarcoma in Texas; all cancer or osteosarcoma in the United Kingdom; osteosarcoma or Ewing sarcoma in Great Britain.

Skeletal effects
Fluoride naturally accumulates in bones. Skeletal fluorosis (changes in bone structure resulting from excess fluoride accumulation) can occur at high levels of fluoride over long periods of time (e.g. over many years). This is known to happen in countries where there are naturally occurring very high concentrations of fluoride in groundwater such as in parts of China, India, and Africa) (see Figure 19). This does not happen with fluoride concentrations in the range experienced by New Zealanders, with or without fluoridation of drinking-water.
In 2014, the Royal Society Te Apārangi concluded that skeletal fluorosis has not been known to occur in Aotearoa New Zealand. This appears to still be accurate; however, a letter to the New Zealand Medical Journal in 2018 proffered one possible case of skeletal fluorosis. High fluoride intake was ascribed to high tea consumption (tea can naturally contain elevated fluoride concentrations), as the case lived in an area with a non-fluoridated water supply. This has not been confirmed nor have other cases been reported in literature.

Acute effects
Most effects discussed for fluoride are based on chronic exposure, e.g. exposure to high levels of fluoride every day for months or years. However, very high one-off exposures to fluoride can be harmful. Acute toxic effects can include nausea, vomiting, abdominal pain, diarrhoea, and weakness. [63] Acute effects are only felt at very high doses so would generally require consumption of a product high in fluoride, for example, consuming whole tubes of toothpaste within a day (see Figure 23) or by consuming a product not meant for human consumption (such as a fluoride-containing insecticide, rodenticide or another industrial product).

Other effects
The most significant concerns and effects are discussed on this webpage, other alleged effects are considered in the Royal Society Te Apārangi review (for example, relating to reproduction, endocrine function, cardiovascular and renal effects, and effects on the immune system). This includes consideration of individuals with kidney disease, as patients with end-stage kidney disease may have elevated blood fluoride concentrations and can be at increased risk of excess fluoride exposure. Chronic kidney disease is common in Aotearoa New Zealand and there is a higher prevalence amongst Māori. However, the most reliable and valid evidence was assessed by Royal Society Te Apārangi for all of these effects and it found that fluoride at levels used for community water fluoridation does not pose significant risks of harm to human health. No significant evidence has arisen that would impact on this conclusion. The Australian review in 2017 found there is reliable evidence that community water fluoridation at current Australian levels is not associated with cancer, Down syndrome, cognitive dysfunction, lowered intelligence or hip fracture. There is no reliable evidence of an association between community water fluoridation at current Australian levels and other human health conditions such as chronic kidney disease, kidney stones, hardening of the arteries (atherosclerosis), high blood pressure, low birth weight, all-cause mortality, musculoskeletal pain, osteoporosis, skeletal fluorosis, thyroid problems, or self-reported ailments such as gastric discomfort, headache, and insomnia.

Fluoride exposure and intake
How much fluoride is appropriate?
Fluoride is absorbed through the gastrointestinal tract and almost all of the fluoride that is retained is stored in the bones and teeth. Children retain much more of the absorbed fluoride than adults (see Figure 12).
Ideal fluoride intake to maximise oral health benefits varies by age, and in adults also varies by sex (see Figure 13) (this is because the recommendation is based on body weight). Nutrient Reference Values are set jointly by the Australian and New Zealand governments. Fluoride is not an essential nutrient but is recommended due to its benefits for oral health.
In setting reference values, the government recommends a level at which fluoride intake is high enough to help prevent dental caries (the ‘adequate intake’), while not being so high as to cause dental fluorosis that is moderate or severe (the ‘upper level’). [64]
The Nutrient Reference Values for infants and children up to eight years old were reviewed and updated in 2017 (see Figure 13).
The reason for this review was that estimates of chronic intake of fluoride for infants were often exceeding the upper levels set (see further information in the section ‘Appropriate fluoride intake in example groups’ below), yet the incidence of moderate dental fluorosis in this age group is rare (and there are no known instances of severe fluorosis in Aotearoa New Zealand). [65] Infant fluoride intake is described further in the section ‘Likely fluoride exposure in example groups’ below.
The change in the estimated values does not have any implication for Aotearoa New Zealand’s drinking standard or for other action related to fluoride intake (e.g. from ingesting fluoride toothpaste).
The values will be reviewed for older children and adults in the future.
The adequate intake values used in Aotearoa New Zealand are broadly similar to those recommended by the United States National Institutes of Health and the European Food Safety Authority (EFSA) [66] (see Figure 14). The EFSA upper levels are consistently set more conservatively than those applied in Australia and Aotearoa New Zealand.

Figure 13: The recommended fluoride intake in Aotearoa New Zealand varies by age and sex. See Nutrient Reference Values set by the Australian and New Zealand Governments.

Figure 12: Retention of absorbed fluoride in adults and infants. See WHO.

Figure 14: Reference values for males in Australia and New Zealand, the United States and Europe.
Appropriate fluoride intake in example groups
Appropriate fluoride intake varies between age groups – examples are given for three different groups below.
Infants aged 7-12 months
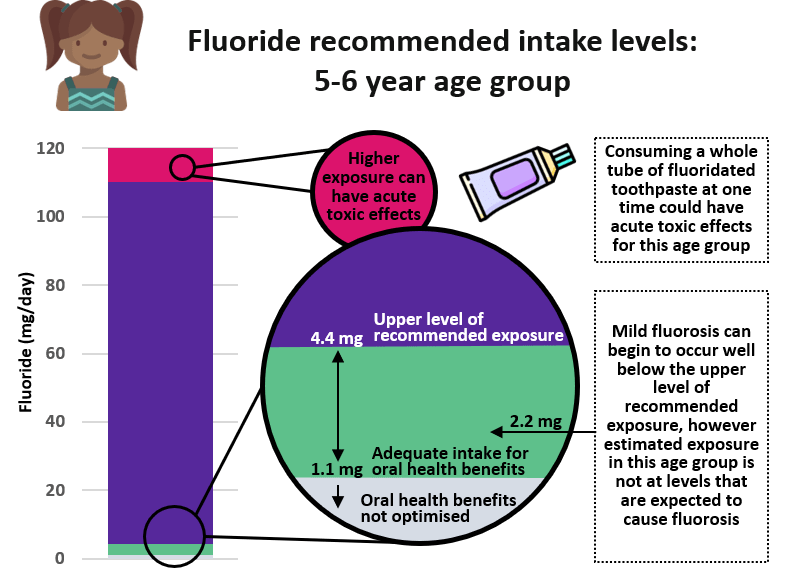
Figure 15 shows the recommended adequate intake levels for infants aged 7-12 months. Due to their small size, infants can consume a relatively small amount of fluoride every day to gain oral health benefits. As covered in the section ‘Likely fluoride exposure in example groups’, infants can be at higher risk of developing mild dental fluorosis from excessive fluoride exposure.
 Figure 15: Recommended fluoride intake levels for infants aged 7-12 months old.
Figure 15: Recommended fluoride intake levels for infants aged 7-12 months old.
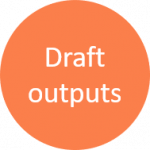
Children aged 5-6 years
Men over 25 years
Figure 17 shows the recommended adequate fluoride intake for men over 25 years old. Adults have the highest recommended intakes due to their larger body size. Men’s estimated intake is explored in [Likely Fluoride exposure in example groups].
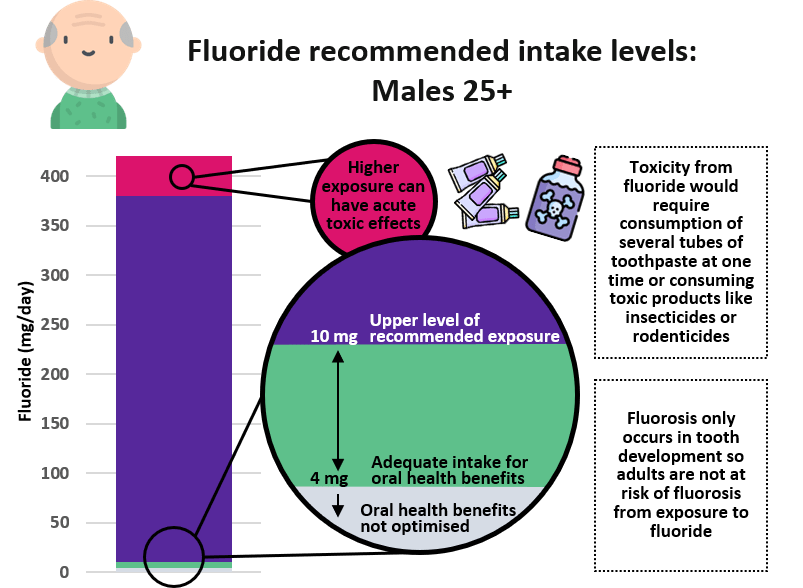 Figure 17: Recommended fluoride intake levels for males over 25 years old.
Figure 17: Recommended fluoride intake levels for males over 25 years old.
What does this mean for fluoridating our water?
While fluoride reference values consider how much fluoride we can safely consume in total each day, when water is fluoridated it is done by checking existing water fluoride levels and adding enough to bring up the water fluoride content to the recommended concentration (how many milligrams per litre). Aotearoa New Zealand fluoridates to reach a level between 0.7 mg and 1.0 mg per litre, which is consistent with recommendations throughout the world. As Figure 18 shows, this range allows the full benefits of fluoride to be achieved while avoiding the adverse impacts that would come with much higher levels of fluoride.

Figure 18: Concentration of fluoride in water and the potential impacts this can have on health.
How much fluoride are we getting and where from?
As well as natural or added fluoride in water supplies, there are other fluoride sources including dietary sources and use of dental products.
Dietary fluoride intake has been previously estimated, in a study by Cressey et al. in 2010 [67] and in estimates produced by Food Standards Australia New Zealand. These studies have recently been outlined and used as reference points by the Australian and New Zealand governments in 2017. These are still the most up-to-date and detailed estimates available, though a recently published thesis presented data on the fluoride intake of adolescents in Aotearoa New Zealand. The research found that most participants did not consume the recommended adequate intake of fluoride, and none exceeded the recommended upper level. The study found that female adolescents in areas that had fluoridated drinking water had four-times the fluoride intake of those in non-fluoridated areas (while males had three-times the fluoride intake). This confirmed similar patterns estimated by Cressey et al., 2010.
Information from Cressey et al., 2010 [68] is drawn on in the figures used here to give examples of fluoride intake in the following groups:
Fluoride intake, and how this compares to recommended intakes, differs widely from group to group.
There have been more recent studies undertaken that look at specific products that affect our overall intake of fluoride.
For example, in recent years non-fluoridated toothpastes have become more widely available (often branded as ‘natural’ toothpastes). People who use non-fluoridated toothpastes rather than fluoridated toothpastes will lower their overall fluoride intake and are potentially at greater risk of dental caries. A cross-sectional study of both adults and children [69] published in 2020, found that the majority of New Zealanders still use fluoridated toothpaste. Around 6-7% of New Zealanders use non-fluoridated toothpaste and usage varied by age, ethnicity and area-level deprivation. Usage of non-fluoridated toothpaste was highest in areas of moderate or low deprivation and for individuals that were of Asian ethnicity. This differs from the groups most at risk from a social equity lens.
A study into the use of full strength toothpaste among preschoolers [70] in Aotearoa New Zealand in 2016 found only around 19% of preschoolers in the sample used full-strength fluoride toothpaste, despite this being recommended for all preschoolers by the Ministry of Health. In recent years many leading toothpaste brands have now removed their low fluoride toothpastes from the Aotearoa New Zealand market, this makes it easier for parents to buy full-strength toothpaste for their children, as recommended by the Ministry of Health for all age groups.

Young child brushing her teeth. © Kyle Alberti.

Older man consuming foods naturally high in fluoride such as black tea, bread, and tinned fish. © Louis Fagan.
In 2017 a study looked at the fluoride level of black tea consumed in Aotearoa New Zealand. [71] The study found that tea is an important source of fluoride consumption in Aotearoa New Zealand. There are no specified regulations concerning fluoride content or labelling in tea products. However, infants, the group at most risk from the negative impacts of fluoride generally do not consume tea. This is explored further for men over 25 years below.
Likely fluoride exposure in example groups
Exposure to fluoride varies between different groups and depends largely on diet.
Men over 25 years
The group with the highest recommended adequate fluoride level is adult men (this is based on an assumed greater mean body weight). This higher recommended intake means that even when water supplies are fluoridated, men may not reach the adequate intake level to maximise oral health benefits from fluoride.
Men over 25 are estimated to get most of their fluoride intake from tea. Where water is fluoridated, instant coffee and water are also large contributors, while beer, bread and carbonated beverages are more important contributors in non-fluoridated areas.
Aotearoa New Zealand has high black tea consumption, but for adult men it could take drinking more than an additional ten large cups of black tea a day to start reaching the upper level of intake for fluoride.
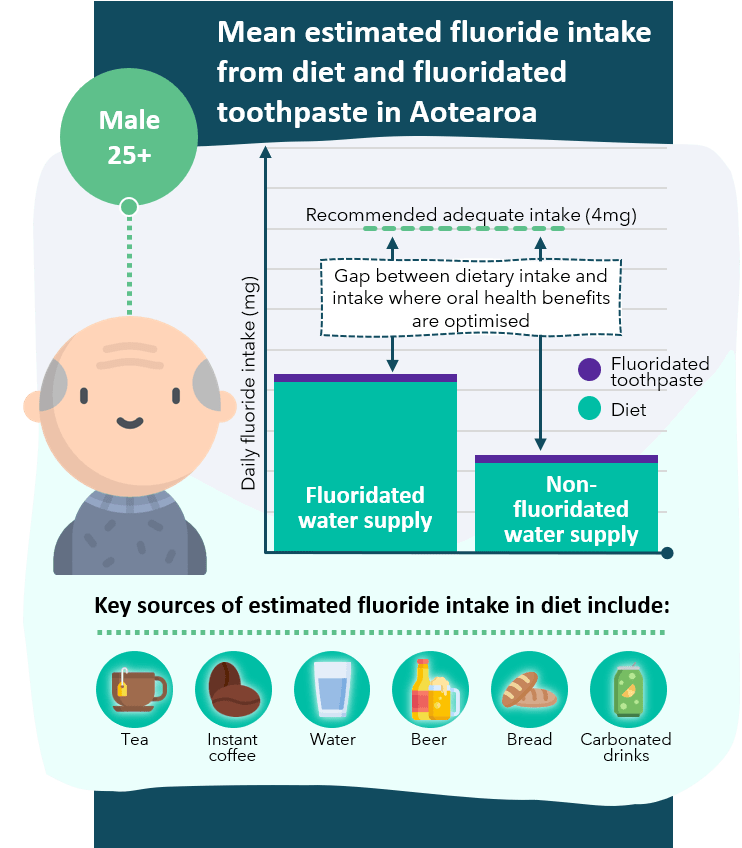 Figure 19: Mean estimated dietary fluoride intake from diet and fluoridated toothpaste in Aotearoa New Zealand for men aged over 25 years old. Data drawn on from Cressey et al.
Figure 19: Mean estimated dietary fluoride intake from diet and fluoridated toothpaste in Aotearoa New Zealand for men aged over 25 years old. Data drawn on from Cressey et al.
Children aged 5-6 years
For children aged 5-6, fluoridating water supplies is a very important contributor to improved oral health.
Children aged between five and six years old are estimated to reach the an adequate intake level for decay prevention where water supplies are fluoridated and fluoridated toothpaste is used. Where water supplies are not fluoridated it is not estimated that this adequate intake level will be reached. So for children aged five to six, fluoridating water supplies is a very important contributor to improved oral health.
Children between five and six years old in fluoridated areas get most of their fluoride intake from water and fruit drink. In non-fluoridated areas, the biggest estimated contributor is bread, while water and other beverages still contribute.
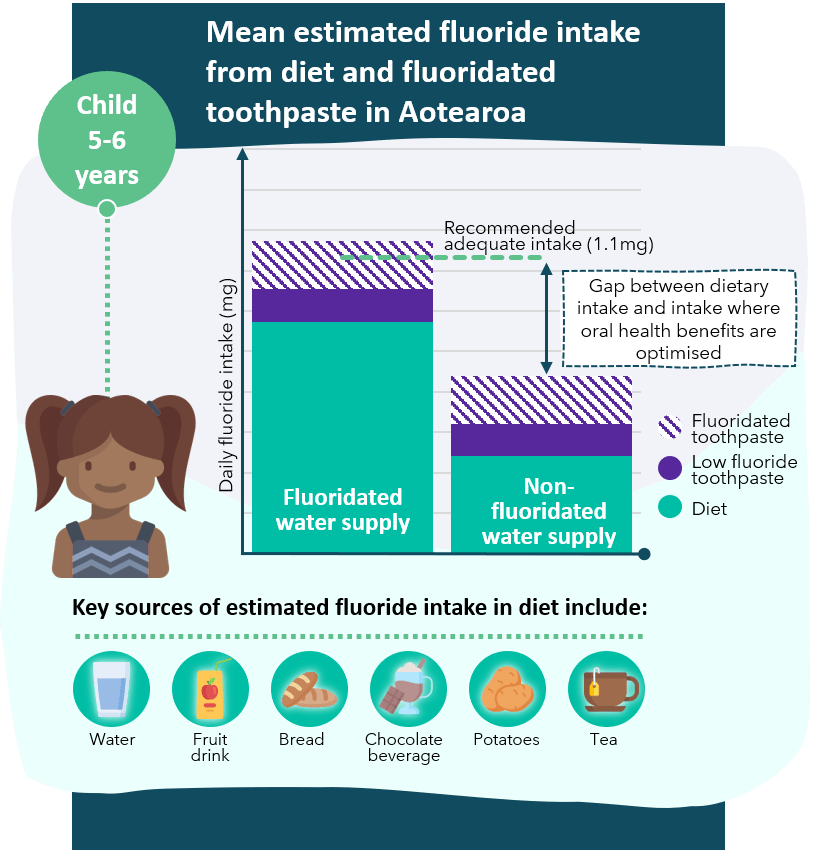 Figure 20: Mean estimated dietary fluoride intake from diet and fluoridated toothpaste in Aotearoa New Zealand for children 5-6 years old. Data drawn on from Cressey et al.
Figure 20: Mean estimated dietary fluoride intake from diet and fluoridated toothpaste in Aotearoa New Zealand for children 5-6 years old. Data drawn on from Cressey et al.
Infants
0-6 months
Formula-fed infants are considered specifically in a paper by Cressey in 2010. [71] Formula-fed babies have a much higher exposure to fluoride than breast-fed babies if fluoridated water is used in preparing formula. Reaching the upper intake level would require a baby to have 1.2 L of formula per day, if the water is fluoridated at 1 mg/L. It is unlikely most babies would drink that much each day, but some could.
7-12 months
Formula-fed babies remain a subset of the population that is most at risk of consuming higher levels of fluoride relative to their body size.
Infants between 7-12 months old get the majority of their fluoride intake from infant formula. This is mainly due to fluoride in the water used in preparing the formula.
Infants that drink fluoridated water are likely to have intakes that are higher than those deemed adequate to maximise oral health benefits, but lower than the upper level of recommended intake. Other contributors include water, infant foods, fruit drink, yoghurt and bread.
The recommended upper level of intake for infants was reviewed and updated in 2017 [link to nutrient reference values table]. In the past, infants who had a diet that included a large quantity of fluoridated water (such as formula-fed babies in areas with a fluoridated water supply) would have intake estimates that may have exceeded the historic recommended upper level. Given that the upper level for this age group has been increased, this is no longer the case. However, formula-fed babies remain a subset of the population that is most at risk of consuming higher levels of fluoride relative to their body size.
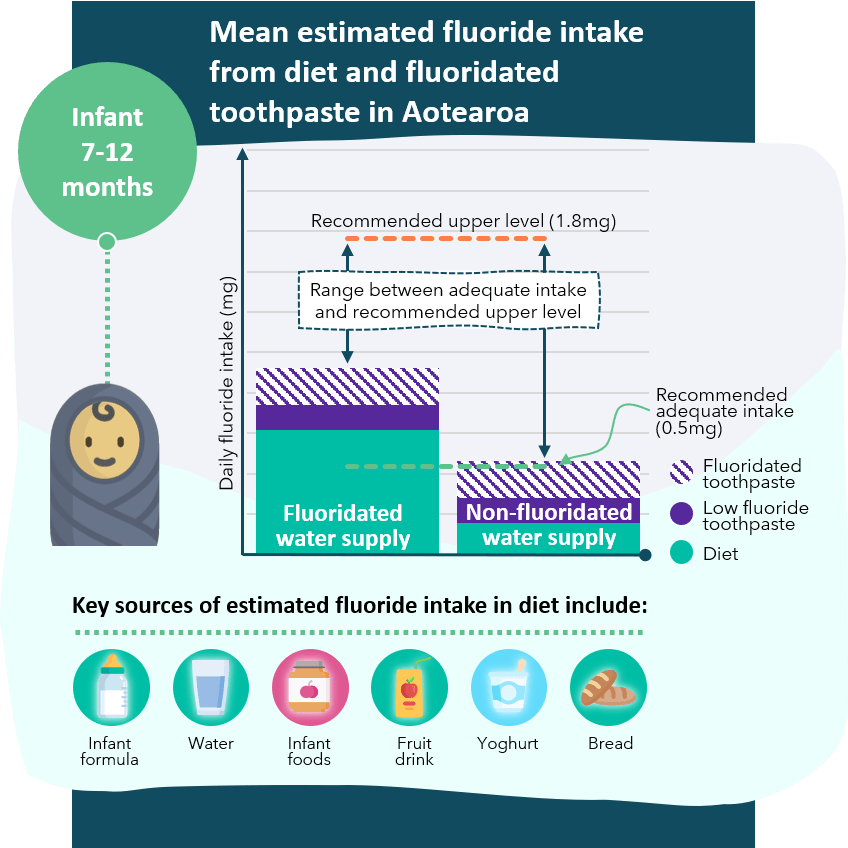 Figure 21: Mean estimated dietary fluoride intake from diet and fluoridated toothpaste in Aotearoa New Zealand for infants 7-12 months old. Data drawn on from Cressey et al.
Figure 21: Mean estimated dietary fluoride intake from diet and fluoridated toothpaste in Aotearoa New Zealand for infants 7-12 months old. Data drawn on from Cressey et al.
Further reading and resources
Neurodevelopmental and cognitive health effects
- Community water fluoridation and intelligence: prospective study in New Zealand (Broadbent et al., 2015) [72] This prospective study found no clear differences in IQ due to fluoride exposure, and that the findings did not support the assertion that fluoride in the context of community water fluoridation programs is neurotoxic. The study postulates that associations between very high fluoride exposure and low IQ reported in previous studies may have been affected by confounding factors, particularly by rural or urban status. The study was also limited in that individual water intake was not measured and dietary fluoride was not considered.
- Prenatal fluoride exposure and cognitive outcomes in children at 4 and 6–12 years of age in Mexico (Bashash et al., 2017) [73] A study of 299 mother-child pairs found that higher prenatal fluoride exposure (in the general range of exposures reported for other general population samples) was associated with lower scores on tests of cognitive function in the children at age 4 and 6–12 years. This study was conducted in an endemic fluoride area (i.e. where fluoride levels are naturally high) and did not consider known potential neurotoxins that could be present in the study area (e.g. arsenic, manganese etc.).
- Association between maternal fluoride exposure during pregnancy and IQ scores in offspring in Canada (Green et al., 2019) [74] A Canadian peer-reviewed study found an association between maternal exposure to higher levels of fluoride during pregnancy and lower IQ scores in their children aged 3 to 4 years. The study had several limitations, which are discussed in detail in [link to section].
- Association between water fluoride and the level of children’s intelligence: a dose-response meta-analysis (Duan et al., 2018) [75] Chinese peer-reviewed meta-analysis that similarly concluded that “greater exposure to high levels of fluoride in water was significantly associated with reduced levels of intelligence in children.”
- Developmental fluoride neurotoxicity: an updated review (Grandjean, 2019) [76] The study concluded that epidemiological results since 2012 support the notion that high exposure to fluoride during early development can result in IQ deficits. The study recommends that neurotoxic risks are recognised when determining the safety of fluoride levels in drinking-water.
- Toxicity of fluoride: critical evaluation of evidence for human developmental neurotoxicity in epidemiological studies, animal experiments and in vitro analyses (Guth et al., 2020) [77] This review concludes that currently available scientific evidence does not support the presumption that fluoride should be assessed as a human developmental neurotoxicant at the current exposure levels in Europe.
- Review of the draft National Toxicology Program (NTP) Monograph on systematic review of fluoride exposure and neurodevelopmental and cognitive health effects (National Academies of Sciences, 2020) [78] This review of the draft undertaken in 2020, found that further analysis or reanalysis is needed to support a conclusion that “fluoride is presumed to be a cognitive neurodevelopmental hazard to humans.”
- Review of the revised NTP Monograph on the systematic review of fluoride exposure and neurodevelopmental and cognitive health effects: A letter (National Academies of Sciences, 2021) [79] This review of the revised draft, undertaken in 2021, suggested that the NTP should make it clear that the monograph could not be used to draw any conclusions regarding low fluoride exposure concentrations (including those typically associated with drinking-water fluoridation) and potential neurodevelopmental and cognitive health effects.
Aotearoa New Zealand exposures and equities
- Estimated dietary fluoride intake for New Zealanders [80] Australian and New Zealand Nutrient Reference Values for Fluoride. See also: Supporting Document 1 Fluoride intake estimates.
- Black tea source, production, and consumption: Assessment of health risks of fluoride intake in New Zealand [81] Aotearoa New Zealand has one of the highest per capita rates of black tea consumption. The study found that tea is an important and underrepresented source of fluoride consumption in Aotearoa New Zealand and is higher than previously recognised. There are no specified regulations concerning fluoride content or labelling in tea products.
- Investigating the prevalence of non-fluoride toothpaste use in adults and children using nationally representative data from New Zealand: a cross-sectional study [82] Around 6-7% of New Zealanders use non-fluoride toothpaste. The highest prevalence of non-fluoride toothpaste use was in the moderate to least-deprived areas. The lowest use was in the most deprived areas. The Asian population had the highest prevalence of use, compared to Māori, Pacific and European/Other.
- Use of full strength fluoride toothpaste among preschoolers in New Zealand, and factors determining toothpaste choice [83] 19% of preschoolers in the sample used full-strength fluoride toothpaste. Parents and caregivers made decisions around purchasing of toothpaste based on the level of trust they had in the brand (59%) and also matching age-specific toothpaste to their child (49%).
- Water fluoridation and ethnic inequities in dental caries profiles of New Zealand children aged 5 and 12–13 years: analysis of national cross-sectional registry databases for the decade 2004–2013 [84] This Aotearoa New Zealand peer-reviewed study explored potential ethnic inequities in dental health. Māori children in areas with community water fluoridation had better oral health profiles than Māori children in non-fluoridated areas; however, Māori children continue to carry a disproportionate oral health burden compared to non-Māori.
- Inequalities in dental caries experience among 4-year-old New Zealand children [85] The study found there were socioeconomic gradients in dental caries experience evident by four years of age. The greatest caries experience and steepest socioeconomic gradients were observed among Māori and Pacific children.
- Area-level deprivation, childhood dental ambulatory sensitive hospitalizations and community water fluoridation: evidence from New Zealand [86]The study found an association between community water fluoridation and reduced avoidable dental-related hospital visits for children aged 0–4 and 5–12 years. The greatest effect of community water fluoridation on reducing rates was found in children living in the most deprived areas. This indicated a greater health gain from community water fluoridation for those with the highest socio-economic disadvantage and so community water fluoridation decisions can contribute to structural inequities in oral-health outcomes for children.
- Association between community water fluoridation and severe dental caries experience in 4-year-old New Zealand children [87] This study found that community water fluoridation continues to be associated with a reduced prevalence of severe dental caries in 4-year-old children in Aotearoa New Zealand. [link back to in-text]
- The costs and benefits of water fluoridation in NZ [88] Ministry of Health funded peer-reviewed study investigated the costs and benefits of water fluoridation in Aotearoa New Zealand. The study concluded that fluoridation of community water supplies remained a highly cost-effective health measure.
- Inequalities in indigenous oral health: findings from Australia, New Zealand, and Canada [89] The study compared differences in the prevalence of Indigenous-related inequalities in dental disease and self-rated oral health in these three countries. In all countries, Indigenous persons had more untreated dental caries and missing teeth, and a higher proportion reporting fair/poor self-rated oral health, than their non-Indigenous counterparts.
Aotearoa New Zealand legislation and guidelines
- Drinking-water Standards for New Zealand 2005 (revised in 2018). The maximum acceptable value (MAV) for fluoride is 1.5 mg/L. For oral health reasons, the Ministry of Health recommends that the fluoride content for drinking water in Aotearoa New Zealand be in the range of 0.7–1.0 mg/L; this is not a MAV. Where fluoridation of a water supply is undertaken, drinking-water leaving the treatment plant must be sampled at a minimum frequency of weekly under the water supplier’s monitoring programme. These standards were deemed to be issued in accordance with Part 2A of the Health Act 1956.
- Water New Zealand Code of Practice Fluoridation of Drinking-Water Supplies in New Zealand. This Code of Practice specifies good practice for the design and operation of water fluoridation plants to ensure the safe and effective addition of fluoride to drinking-water supplies. It is endorsed by the Ministry of Health as representing good practice for the addition of fluoride to drinking water for the promotion of dental health. Compliance with the Code of Practice is not a legal requirement but is a way to provide increased public confidence.
- Health Act 1956. Under part 2A (Drinking Water) of the Act, territorial authorities The Minister may issue or adopt standards for drinking water, but must not include any requirement that fluoride be added to drinking water (section 69O). Under Section 23 of the Act, local authorities have the duty to “improve, promote, and protect public health within its district”. Other relevant provisions are found under Sections 3A and 27A of the Act.
- Health (Fluoridation of Drinking Water) Amendment Bill. The Health (Fluoridation of Drinking Water) Amendment Bill was introduced in November 2016 and is currently awaiting its second reading. The bill would amend Part 2A of the Health Act 1956 by empowering the Director General of Health to decide and direct territorial authorities to fluoridate or not fluoridate drinking water supplies in their areas (territorial authorities currently make this decision). See also the Regulatory Impact Statement and Cabinet Paper.
- Drinking-water fluoridation subsidy. District councils can apply to the Ministry of Health for financial assistance with the set-up costs of water fluoridation.
- Australian and New Zealand Nutrient Reference Values for Fluoride. A report prepared for the Australian Government Department of Health and the New Zealand Ministry of Health.
Recent international government reviews
Australian review
- In 2017, the Australian National Health and Medical Research Council (NHMRC) released a number of documents related to the health effects of water fluoridation.
- NHMRC Public Statement 2017
- Information paper – water fluoridation: dental and other human health outcomes [90]
- Health effects of water fluoridation – evidence evaluation report [91]
- Health effects of water fluoridation – technical report [92]
- Evaluating the evidence on water fluoridation and human health in Australia 2014-2017 – Administrative Report [93]
- The NHMRC public statement in 2017 states: “NHMRC strongly recommends community water fluoridation as a safe, effective and ethical way to help reduce tooth decay across the population. NHMRC supports Australian states and territories fluoridating their drinking water supplies within the range of 0.6 to 1.1 milligrams per litre (mg/La).”
- Key findings of the review include:
- Tooth decay. Water fluoridation reduces tooth decay in children and adolescents by 26% to 44%, and by 27% in adults.
- Dental fluorosis. Almost all dental fluorosis occurring in Australia is very mild or mild, doesn’t affect the function of the teeth, and is not of aesthetic concern to those who have it. Dental fluorosis that is very mild or mild has been associated with a protective benefit against tooth decay in adults. In Australia, moderate dental fluorosis is very uncommon and severe dental fluorosis is rare. There is no evidence that community water fluoridation at Australian levels gives rise to these forms of dental fluorosis, as the incidence is not statistically different between fluoridated and non-fluoridated areas. Dental fluorosis declined over the time in which fluoridation of community water in Australia expanded. The decline is linked to reduced exposure to fluoride from other sources (e.g. availability and promotion of low fluoride toothpaste for children, public health messages and guidelines about use of the products).
- Other effects. There is reliable evidence that community water fluoridation at current Australian levels is not associated with cancer, Down syndrome, cognitive dysfunction, lowered intelligence or hip fracture. There is no reliable evidence of an association between community water fluoridation at current Australian levels and other human health conditions such as chronic kidney disease, kidney stones, hardening of the arteries (atherosclerosis), high blood pressure, low birth weight, all-cause mortality, musculoskeletal pain, osteoporosis, skeletal fluorosis, thyroid problems or self-reported ailments such as gastric discomfort, headache, and insomnia.
Europe
- Critical review of any new evidence on the hazard profile, health effects, and human exposure to fluoride and the fluoridating agents of drinking water. European Union 2011: Scientific Committee on Health and Environmental Risks.
- Health effects of water fluoridation: An evidence review 2015. Health Research Board of Ireland. This review found no strong evidence that community water fluoridation is definitely associated with negative health effects. the review did find there are strong suggestions that high levels of naturally occurring fluoride in water may be associated with negative health effects, in particular, skeletal fluorosis and lowering of IQ. The evidence base for this association comes mainly from low quality studies of inappropriate study design. See also the FACCT study that took place in Ireland, which assessed the impact of changes in fluoridation of drinking-water on tooth decay and dental fluorosis levels in children.
- The effects of fluoride in drinking water. [94] A retrospective cohort study conducted by the Institute for Evaluation of Labour Market and Education Policy (IFAU), a research institute under the Swedish Ministry of Employment. A zero effect on cognitive ability was reported. The positive effect of fluoride on dental health was also confirmed.
- Scientific opinion on dietary reference values for fluoride. European Food Safety Authority (EFSA) Panel on dietetic products, nutrition, and Allergies (NDA). While fluoride is not an essential nutrient, the Panel considered that setting an Adequate Intake level was appropriate because of the beneficial effects of dietary fluoride on prevention of dental caries.
- Dental care and water fluoridation. Public Health England report (2018).
Canada
- CADTH (Canadian Agency for Drugs and Technologies in Health) Rapid response report: Summary with critical appraisal. Community Water Fluoridation Exposure: A Review of Neurological and Cognitive Effects [95] This review identified one prospective birth cohort study examining the association between fluoride exposure of mothers during pregnancy and subsequent children’s intelligence quotient (IQ) scores (see section ‘Neurodevelopmental and cognitive health effects’). The review finds the interaction between child sex and maternal fluoride intake was not statistically significant, the evidence is weak due to multiple limitations, and that the findings of this study should be interpreted with caution.
- Update: CADTH Rapid response report: Summary with critical appraisal. Community Water Fluoridation Exposure: A Review of Neurological and Cognitive Effects – A 2020 Update The review included one prospective cohort study and two cross-sectional studies examining the effect of fluoride exposure on IQ and attention deficit hyperactivity disorder (ADHD) diagnosis in children. These studies were considered to be of low quality due to high risk of bias and multiple limitations. Considering multiple limitations of the included studies (e.g., insufficient control of confounding factors, potential misclassification of exposure, and inadequate study design), the review found it difficult to interpret their findings and generalise them to the Canadian context. The review concludes that “collective evidence from the recent CADTH reports and the current review indicates there is insufficient evidence to conclusively conclude that fluoride exposure at the Canadian water fluoride levels (optimum at 0.7 mg/L) affects neurological development in children and adolescents in Canada.”
- See also: CADTH Technology review. Community Water Fluoridation Programs: A Health Technology Assessment — Review of Dental Caries and Other Health Outcomes [96]
- Public Health Ontario, Canada: Evidence Review for Adverse Health Effects of Drinking Optimally Fluoridated Water (2010- 2017) [97] The review finds existing literature (to May 2017) indicates that mild dental fluorosis (generally unnoticeable white specks on teeth) is the only adverse effect experienced from the consumption of optimally fluoridated water. However, infant formulas mixed with optimally fluoridated water may increase the chance of mild dental fluorosis if it is the child’s main food source. If prevention of the mild fluorosis is desired then infant formula can be occasionally mixed with low-fluoridated bottled water and early exposure to other forms of fluoride including fluoride toothpaste, fluoride rinse, and fluoride supplements should be monitored.
United States (draft materials)
- The recent draft materials are discussed above in the section ‘US review of evidence: Ongoing review process of draft outputs on neurodevelopmental and cognitive health effects’. Documents include:
- Draft National Toxicology Program (NTP) Monograph on systematic review of fluoride exposure and neurodevelopmental and cognitive health effects, revised September 16 2020 [98]
- Review of the draft National Toxicology Program (NTP) Monograph on systematic review of fluoride exposure and neurodevelopmental and cognitive health effects [99]
- Review of the revised NTP Monograph on the systematic review of fluoride exposure and neurodevelopmental and cognitive health effects: A letter [100]
- Literature search results for the systematic review of fluoride exposure and neurodevelopmental and cognitive health effects [101]
- American Dental Association re revised NTP Monograph on fluoride exposure and neurodevelopmental and cognitive health October 16 2020
Aotearoa New Zealand
- Royal Society Te Apārangi 2014 comprehensive review of health effects of water fluoridation [102]. The review found that there were no adverse effects of fluoride of any significance arising from fluoridation at the levels used in Aotearoa New Zealand.
Other resources
- ESR list of fluoridated water supplies
- WHO monograph on fluoride in drinking-water, which focuses on the prevention of adverse effects from excessive levels of fluoride in drinking water.
Peer reviewers
We extend our thanks to our peer reviewers for providing comment and feedback on draft materials.
- Dr Anne Bardsley. Deputy Director, Koi Tū: Centre for Informed Futures, main writer of 2014 Royal Society Te Apārangi fluoride review.
- Associate Professor Jonathan Broadbent. Longitudinal dental health research, Dental Public Health. University of Otago.
- Dr Riana Clarke. National Clinical Director Oral Health. Dentist. Ministry of Health.
- Peter Cressey. Senior Scientist at ESR.
- Dr Belinda Cridge. Mechanistic toxicologist. Technical Lead, Drinking Water at ESR. University of Otago.
- Professor Mark J Ferguson. Director General and Chief Scientific Adviser to the Government of Ireland, Science Foundation Ireland.
- Dr Sabine Guth. rer. nat. DFG-Senate Commission on Food Safety (DFG-SKLM) Scientific Office, Leibniz Research Centre, Germany.
- Professor Jan Hengstler. Head of Department, Toxicology, Leibniz Research Centre (IfADo), Leibniz Research Centre, Germany.
- Dr Tule Fanakava Misa. Public health dentist, President NZ Society of Hospital and Community Dentistry, CDHB.
- Professor Sir David Skegg. Emeritus Professor, Epidemiology and public health, author of 2014 Royal Society Te Apārangi fluoride review, University of Otago.
- Dr Moira Smith. BDS PhD PGDipSci DPH. Senior Research Fellow and Senior Lecturer, Co-Director, HePPRU: Health Promotion and Policy Research Unit, Department of Public Health, University of Otago.
- Dr Justin Wall. BDS, DPH, Dip.Clin.Dent. Chair, Māori Oral Health Quality Improvement Group.
Footnotes
[1] Formerly known as the Royal Society of New Zealand.
[2] Gluckman et al., “Health Effects of Water Fluoridation: A Review of the Scientific Evidence. A Report on Behalf of the Royal Society of New Zealand and the Office of the Prime Minister’s Chief Science Advisor”, 2014.
[3] Gluckman et al., “Health Effects of Water Fluoridation: A Review of the Scientific Evidence. A Report on Behalf of the Royal Society of New Zealand and the Office of the Prime Minister’s Chief Science Advisor”, 2014.
[4] Awofeso, “Ethics of Artificial Water Fluoridation in Australia,” Public Health Ethics 5, no. 2 (2012).
[5] Jiang et al., “Is New Zealand Water Fluoridation Justified?,” New Zealand Medical Journal 127, no. 1406 (2014).
[6] Song et al., “Community Water Fluoridation: Caveats to Implement Justice in Public Oral Health,” International Journal of Environmental Research and Public Health 18, no. 5 (2021).
[7] Ministry of Health, “Our Oral Health: Key Findings of the 2009 New Zealand Oral Health Survey”, 2010.
[8] Ministry of Health, “Reducing Inequalities in Health”, 2002.
[9] 45.1%.
[10] Aung et al., “Dental Caries and Previous Hospitalisations among Preschool Children: Findings from a Population-Based Study in New Zealand,” New Zealand Medical Journal 132, no. 1493 (2019).
[11] Johnston et al., “Principles of Fluoride Toxicity and the Cellular Response: A Review,” Archives of Toxicology 94, no. 4 (2020).
[12] Götzfried, “Legal Aspects of Fluoride in Salt, Particularly within the EU,” Schweiz Monatsschr Zahnmed 116, no. 4 (2006).
[13] Marthaler, “Overview of Salt Fluoridation in Switzerland since 1955, a Short History,” Schweiz Monatsschr Zahnmed 115, no. 8 (2005).
[14] Schulte, “Salt Fluoridation in Germany since 1991,” Schweiz Monatsschr Zahnmed 115, no. 8 (2005).
[15] Tramini, “Salt Fluoridation in France since 1986,” Schweiz Monatsschr Zahnmed 115, no. 8 (2005).
[16] Cantoral et al., “Fluoride Content in Foods and Beverages from Mexico City Markets and Supermarkets,” Food and Nutrition Bulletin 40, no. 4 (2019).
[17] Kimambo et al., “Fluoride Occurrence in Groundwater Systems at Global Scale and Status of Defluoridation – State of the Art,” Groundwater for Sustainable Development 9 (2019).
[18] Most areas of Aotearoa New Zealand have natural fluoride levels between 0.1 and 0.2 mg/L, the highest known naturally occurring natural levels of fluoride in groundwater are approximately 0.56 mg/L. Gluckman et al., “Health Effects of Water Fluoridation: A Review of the Scientific Evidence. A Report on Behalf of the Royal Society of New Zealand and the Office of the Prime Minister’s Chief Science Advisor”, 2014.
[19] Moore et al., “The Costs and Benefits of Water Fluoridation in NZ” BMC Oral Health 17, no. 1 (2017).
[20] Moore et al., “The Costs and Benefits of Water Fluoridation in NZ” BMC Oral Health 17, no. 1 (2017).
[21] National Health and Medical Research Council, “Evaluating the Evidence on Water Fluoridation and Human Health in Australia 2014-2017: Administrative Report.” 2017.
[22] Moore et al., “The Costs and Benefits of Water Fluoridation in NZ” BMC Oral Health 17, no. 1 (2017).
[23] Gluckman et al., “Health Effects of Water Fluoridation: A Review of the Scientific Evidence. A Report on Behalf of the Royal Society of New Zealand and the Office of the Prime Minister’s Chief Science Advisor”, 2014.
[24] Schluter et al., “Water Fluoridation and Ethnic Inequities in Dental Caries Profiles of New Zealand Children Aged 5 and 12–13 Years: Analysis of National Cross-Sectional Registry Databases for the Decade 2004–2013,” BMC Oral Health 16, no. 1 (2016).
[25] Note socio-economic status was not measured and could have a confounding effect that has not been accounted for in this study.
[26] Gibb et al., “How Universal Are Universal Preschool Health Checks? An Observational Study Using Routine Data from New Zealand’s B4 School Check,” BMJ Open 9, no. 4 (2019).
[27] Shackleton et al., “Inequalities in Dental Caries Experience among 4-Year-Old New Zealand Children,” Community Dentistry And Oral Epidemiology 46, no. 3 (2018).
[28] Schluter et al., “Association between Community Water Fluoridation and Severe Dental Caries Experience in 4-Year-Old New Zealand Children,” JAMA Pediatrics 174, no. 10 (2020).
[29] Schluter et al., “Association between Community Water Fluoridation and Severe Dental Caries Experience in 4-Year-Old New Zealand Children,” JAMA Pediatrics 174, no. 10 (2020).
[30] Hobbs et al., “Area-Level Deprivation, Childhood Dental Ambulatory Sensitive Hospitalizations and Community Water Fluoridation: Evidence from New Zealand,” International Journal of Epidemiology 49, no. 3 (2020).
[31] Jamieson et al., “Inequalities in Indigenous Oral Health: Findings from Australia, New Zealand, and Canada,” Journal of Dental Research 95, no. 12 (2016).
[32] Moffat et al., “New Zealand’s School Dental Service over the Decades: Its Response to Social, Political, and Economic Influences, and the Effect on Oral Health Inequalities,” Frontiers in public health 5 (2017).
[33] Moore et al., “The Costs and Benefits of Water Fluoridation in NZ” BMC Oral Health 17, no. 1 (2017).
[34] Whyman et al., “Community Water Fluoridation: Attitudes and Opinions from the New Zealand Oral Health Survey,” Australian and New Zealand Journal of Public Health 40, no. 2 (2016).
[35] For example, see current challenges in England. Furness et al., “Water Fluoridation: Current Challenges,” Archives of Disease in Childhood (2020).
[36] Carstairs, “Debating Water Fluoridation before Dr. Strangelove,” American Journal of Public Health 105, no. 8 (2015).
[37] Aoun et al., “The Fluoride Debate: The Pros and Cons of Fluoridation,” Preventive Nutrition and Food Science 23, no. 3 (2018).
[38] Gilpin et al., “A Large Scale Waterborne Campylobacteriosis Outbreak, Havelock North, New Zealand,” Journal of Infection 81, no. 3 (2020).
[39] Gluckman et al., “Health Effects of Water Fluoridation: A Review of the Scientific Evidence. A Report on Behalf of the Royal Society of New Zealand and the Office of the Prime Minister’s Chief Science Advisor”, 2014.
[40] Gluckman et al., “Health Effects of Water Fluoridation: A Review of the Scientific Evidence. A Report on Behalf of the Royal Society of New Zealand and the Office of the Prime Minister’s Chief Science Advisor”, 2014.
[41] Gluckman et al., “Health Effects of Water Fluoridation: A Review of the Scientific Evidence. A Report on Behalf of the Royal Society of New Zealand and the Office of the Prime Minister’s Chief Science Advisor”, 2014.
[42] Ministry of Health, “Our Oral Health: Key Findings of the 2009 New Zealand Oral Health Survey”, 2010.
[43] Note it is also possible for there to be misdiagnosis whereby dental fluorosis might be mistaken for other teeth conditions (such as physical during tooth development) or vice versa.
[44] Gluckman et al., “Health Effects of Water Fluoridation: A Review of the Scientific Evidence. A Report on Behalf of the Royal Society of New Zealand and the Office of the Prime Minister’s Chief Science Advisor”, 2014.
[45] i.e. Chronic exposure at 100 times higher levels than humans would likely be exposed to in Aotearoa New Zealand.
[46] Gluckman et al., “Health Effects of Water Fluoridation: A Review of the Scientific Evidence. A Report on Behalf of the Royal Society of New Zealand and the Office of the Prime Minister’s Chief Science Advisor”, 2014.
[47] Broadbent et al., “Community Water Fluoridation and Intelligence: Prospective Study in New Zealand,” American Journal of Public Health 105, no. 1 (2015).
[48] Bashash et al., “Prenatal Fluoride Exposure and Cognitive Outcomes in Children at 4 and 6-12 Years of Age in Mexico,” Environmental Health Perspectives 125, no. 9 (2017).
[49] Yu et al., “Threshold Effects of Moderately Excessive Fluoride Exposure on Children’s Health: A Potential Association between Dental Fluorosis and Loss of Excellent Intelligence,” Environment International 118 (2018).
[50] Green et al., “Association between Maternal Fluoride Exposure During Pregnancy and Iq Scores in Offspring in Canada,” JAMA Pediatrics 173, no. 10 (2019).
[51] Guth et al., “Toxicity of Fluoride: Critical Evaluation of Evidence for Human Developmental Neurotoxicity in Epidemiological Studies, Animal Experiments and in Vitro Analyses,” Archives of Toxicology 94, no. 5 (2020).
[52] A confounding factor is a variable that isn’t accounted for in a study and that could have caused the results seen in the study (rather than the factors being examined).
[53] Green et al., “Association between Maternal Fluoride Exposure During Pregnancy and IQ Scores in Offspring in Canada” JAMA Pediatrics 173, no. 10 (2019).
[54] A 1 mg/L increase in maternal urinary fluoride was associated with a 4.49-point lower IQ score (95% CI, -8.38 to -0.60) in boys.
[55] Note this is not to say that there might not be a sex-based difference, however there is no detailed explanation provided in the article.
[56] Green et al., “Association between Maternal Fluoride Exposure During Pregnancy and IQ Scores in Offspring in Canada” JAMA Pediatrics 173, no. 10 (2019).
[57] Broadbent et al., “Community Water Fluoridation and Intelligence: Prospective Study in New Zealand” American Journal of Public Health 105, no. 1 (2015).
[58] Guth et al., “Toxicity of Fluoride: Critical Evaluation of Evidence for Human Developmental Neurotoxicity in Epidemiological Studies, Animal Experiments and in Vitro Analyses,” Archives of Toxicology 94, no. 5 (2020).
[59] Guth et al., “Toxicity of Fluoride: Critical Evaluation of Evidence for Human Developmental Neurotoxicity in Epidemiological Studies, Animal Experiments and in Vitro Analyses,” Archives of Toxicology 94, no. 5 (2020).
[60] The measure of IQ was more complete and rigorous, included subscale, and was measured at multiple ages.
[61] Broadbent et al., “Community Water Fluoridation and Intelligence: Prospective Study in New Zealand,” American Journal of Public Health 105, no. 1 (2015).
[62] Ullah et al., “Potential Fluoride Toxicity from Oral Medicaments: A Review,” Iran Journal of Basic Medical Sciences 20, no. 8 (2017).
[63] Australian Government Department of Health and New Zealand Ministry of Health, “Australian and New Zealand Nutrient Reference Values for Fluoride. A Report Prepared for the Australian Government Department of Health and the New Zealand Ministry of Health.”, 2017.
[64] Australian Government Department of Health and New Zealand Ministry of Health, “Australian and New Zealand Nutrient Reference Values for Fluoride. A Report Prepared for the Australian Government Department of Health and the New Zealand Ministry of Health.”, 2017.
[65] European Food Safety Authority, “Dietary Reference Values for Nutrients. Summary Report”, 2019.
[66] Cressey et al., “Estimated Dietary Fluoride Intake for New Zealanders,” Journal of Public Health Dentistry 70, no. 4 (2010).
[67] Cressey et al., “Estimated Dietary Fluoride Intake for New Zealanders,” Journal of Public Health Dentistry 70, no. 4 (2010).
[68] Hobbs et al., “Investigating the Prevalence of Non-Fluoride Toothpaste Use in Adults and Children Using Nationally Representative Data from New Zealand: A Cross-Sectional Study,” British Dental Journal 228, no. 4 (2020).
[69] Li et al., “Use of Full Strength Fluoride Toothpaste among Preschoolers in New Zealand, and Factors Determining Toothpaste Choice,” New Zealand Medical Journal 129, no. 1436 (2016).
[70] Waugh et al., “Black Tea Source, Production, and Consumption: Assessment of Health Risks of Fluoride Intake in New Zealand,” Journal of Environmental and Public Health 2017 (2017).
[71] Cressey, “Dietary Fluoride Intake for Fully Formula-Fed Infants in New Zealand: Impact of Formula and Water Fluoride,” Journal of Public Health Dentistry 70, no. 4 (2010).
[72] Broadbent et al., “Community Water Fluoridation and Intelligence: Prospective Study in New Zealand,” American Journal of Public Health 105, no. 1 (2015).
[73] Bashash et al., “Prenatal Fluoride Exposure and Cognitive Outcomes in Children at 4 and 6-12 Years of Age in Mexico,” Environmental Health Perspectives 125, no. 9 (2017).
[74] Green et al., “Association between Maternal Fluoride Exposure During Pregnancy and IQ Scores in Offspring in Canada,” JAMA Pediatrics 173, no. 10 (2019).
[75] Duan et al., “Association between Water Fluoride and the Level of Children’s Intelligence: A Dose-Response Meta-Analysis,” Public Health 154 (2018).
[76] Grandjean, “Developmental Fluoride Neurotoxicity: An Updated Review,” Environmental Health 18, no. 1 (2019).
[77] Guth et al., “Toxicity of Fluoride: Critical Evaluation of Evidence for Human Developmental Neurotoxicity in Epidemiological Studies, Animal Experiments and in Vitro Analyses,” Archives of Toxicology 94, no. 5 (2020).
[78] National Academies of Sciences, “Review of the Draft NTP Monograph Systematic Review of Fluoride Exposure and Neurodevelopmental and Cognitive Health Effects”, 2020.
[79] National Academies of Sciences, Review of the Revised NTP Monograph on the Systematic Review of Fluoride Exposure and Neurodevelopmental and Cognitive Health Effects: A Letter Report (Washington, DC: The National Academies Press, 2021).
[80] Cressey et al., “Estimated Dietary Fluoride Intake for New Zealanders,” Journal of Public Health Dentistry 70, no. 4 (2010).
[81] Waugh et al., “Black Tea Source, Production, and Consumption: Assessment of Health Risks of Fluoride Intake in New Zealand,” Journal of Environmental and Public Health 2017 (2017).
[82] Hobbs et al., “Investigating the Prevalence of Non-Fluoride Toothpaste Use in Adults and Children Using Nationally Representative Data from New Zealand: A Cross-Sectional Study,”
[83] Li et al., “Use of Full Strength Fluoride Toothpaste among Preschoolers in New Zealand, and Factors Determining Toothpaste Choice,” New Zealand Medical Journal 129, no. 1436 (2016).
[84] Schluter et al., “Water Fluoridation and Ethnic Inequities in Dental Caries Profiles of New Zealand Children Aged 5 and 12–13 Years: Analysis of National Cross-Sectional Registry Databases for the Decade 2004–2013,” JAMA Pediatrics 174, no. 10 (2020).
[85] Shackleton et al., “Inequalities in Dental Caries Experience among 4-Year-Old New Zealand Children,” Community Dentistry And Oral Epidemiology 46, no. 3 (2018).
[86] Hobbs et al., “Area-Level Deprivation, Childhood Dental Ambulatory Sensitive Hospitalizations and Community Water Fluoridation: Evidence from New Zealand,” British Dental Journal 228, no. 4 (2020).
[87] Schluter et al., “Association between Community Water Fluoridation and Severe Dental Caries Experience in 4-Year-Old New Zealand Children,” JAMA Pediatrics 174, no. 10 (2020).
[88] Moore et al., “The Costs and Benefits of Water Fluoridation in NZ,” BMC Oral Health 17, no. 1 (2017).
[89] Jamieson et al., “Inequalities in Indigenous Oral Health: Findings from Australia, New Zealand, and Canada,” Journal of Dental Research 95, no. 12 (2016).
[90] National Health and Medical Research Council, “Evaluating the Evidence on Water Fluoridation and Human Health in Australia 2014-2017: Administrative Report.” 2017.
[91] Jack et al., “Health Effects of Water Fluoridation: Evidence Evaluation Report, Report to the National Health and Medical Research Council”, 2016.
[92] Jack et al., “Health Effects of Water Fluoridation: Technical Report, Report to the National Health and Medical Research Council”, 2016.
[93] National Health and Medical Research Council, “Evaluating the Evidence on Water Fluoridation and Human Health in Australia 2014-2017: Administrative Report”, 2017.
[94] Aggeborn et al., “The Effects of Fluoride in Drinking Water,” Journal of Political Economy 129, no. 2 (2020).
[95] Canadian Agency for Drugs and Technologies in Health (CADTH), “Community Water Fluoridation: A Review of Neurological and Cognitive Effects”, 2019.
[96] Canadian Agency for Drugs and Technologies in Health (CADTH), “Community Water Fluoridation Programs: A Health Technology Assessment — Review of Dental Caries and Other Health Outcomes”, 2019.
[97] Ontario Agency for Health Protection and Promotion (Public Health Ontario), “Evidence Review for Adverse Health Effects of Drinking Optimally Fluoridated Water: Evidence since the 2010 Health Canada Fluoride Document”, 2018.
[98] National Toxicology Program, “Draft NTP Monograph on the Systematic Review of Fluoride Exposure and Neurodevelopmental Cognitive Health Effects, Revised September 16, 2020.”, 2020.
[99] National Academies of Sciences, “Review of the Draft NTP Monograph Systematic Review of Fluoride Exposure and Neurodevelopmental and Cognitive Health Effects”, 2020
[100] National Academies of Sciences, Review of the Revised NTP Monograph on the Systematic Review of Fluoride Exposure and Neurodevelopmental and Cognitive Health Effects: A Letter Report.
[101] National Toxicology Program, “Literature Search Results for the Systematic Review of Fluoride Exposure and Neurodevelopmental and Cognitive Health Effects”, 2020.
[102] Gluckman et al., “Health Effects of Water Fluoridation: A Review of the Scientific Evidence. A Report on Behalf of the Royal Society of New Zealand and the Office of the Prime Minister’s Chief Science Advisor”, 2014.
Last updated: 21 September 2021